Cvs Caremark Prior Authorization Form
Are you familiar with the CVS Caremark Prior Authorization Form? This important document plays a crucial role in the healthcare industry, ensuring that patients receive the medications they need while also controlling costs for both patients and insurance providers. In this blog post, we will explore the purpose of the Prior Authorization Form, why it is necessary, and how it can benefit both patients and healthcare providers. We will also guide you through the process of obtaining and filling out the form, as well as the expected results and benefits of using it. Whether you’re a patient navigating the complexities of the healthcare system or a healthcare professional looking to streamline the medication approval process, understanding and utilizing the CVS Caremark Prior Authorization Form is essential. Let’s dive in and explore this important aspect of medication management.
What is a Prior Authorization Form?
Prior Authorization Forms are documents used by insurance companies to determine if they will cover a specific prescription medication, medical procedure, or service. These forms are typically required for medications that are not on the insurer’s list of preferred drugs, or for treatments that are not considered standard care. The purpose of the form is to ensure that the medication or service is medically necessary and cost-effective. It is a way for insurance companies to manage costs and regulate the use of certain treatments.
Patients or their healthcare providers are usually responsible for requesting prior authorization from the insurance company. The process involves submitting the necessary medical information and documentation to support the need for the medication or treatment. Once the insurance company reviews the request, they will either approve or deny the prior authorization.
If the prior authorization is approved, the insurance company will cover the cost of the medication or procedure. If it is denied, the patient or healthcare provider may have the option to appeal the decision or seek alternative treatment options. Prior Authorization Forms are an essential part of the healthcare system, as they help ensure that patients receive the most appropriate and cost-effective care.
It’s important for patients and healthcare providers to understand the specific requirements and guidelines of their insurance company when it comes to prior authorization. This includes knowing which medications or services require prior authorization, how to submit the necessary paperwork, and the potential outcomes of the approval process.
Reasons for Using Cvs Caremark Prior Authorization Form
Obtaining Cvs Caremark Prior Authorization Form is essential for a number of reasons. One of the main benefits of using this form is to ensure that patients receive the proper medication prescribed by their healthcare provider. By requiring prior authorization for certain medications, Cvs Caremark can review the medication to determine its necessity and appropriateness for the patient’s condition. This helps to lower the risk of misuse or overuse of certain medications, ultimately leading to better patient outcomes and improved quality of care.
Another reason for using the Cvs Caremark Prior Authorization Form is to control healthcare costs. With the rising cost of medications and healthcare services, it’s important for healthcare providers and pharmacy benefit managers to have measures in place to ensure that resources are used efficiently. The prior authorization process can help identify more cost-effective treatment options or alternatives to expensive medications, ultimately benefiting both the patient and the healthcare system as a whole.
Furthermore, the use of Cvs Caremark Prior Authorization Form can help prevent medication errors. By reviewing each medication before it is dispensed, the prior authorization process can help catch any potential errors or issues with the prescription, such as drug interactions or contraindications. This helps to reduce the risk of adverse drug effects and improve patient safety.
Finally, using the Cvs Caremark Prior Authorization Form can help streamline the medication approval process. By providing the necessary information and documentation upfront, healthcare providers can avoid delays in getting patients the medications they need. This can ultimately lead to quicker access to essential medications and improved patient satisfaction.
How to Obtain Cvs Caremark Prior Authorization Form
When it comes to obtaining a Cvs Caremark Prior Authorization Form, there are several options available to ensure that you can access this important document. The first and most straightforward method is to visit the official website of Cvs Caremark. Once on the website, you can navigate to the appropriate section and fill out the necessary information. This will allow you to download the form directly to your computer or print it out for immediate use.
If you prefer to obtain the form in person, you can visit a local Cvs pharmacy location. Most Cvs pharmacies will have physical copies of the prior authorization form available for patients to pick up. Simply ask the pharmacist for the form and they will be able to provide it to you.
For those who prefer to handle things over the phone, you can contact the Cvs Caremark customer service hotline. A representative will be able to assist you in obtaining the prior authorization form and can also address any questions or concerns you may have about the process.
Regardless of the method you choose, it’s important to have a Cvs Caremark Prior Authorization Form on hand if you’re planning to use Cvs Caremark for your prescription drug coverage. By following these simple steps, you can easily obtain the form and ensure that you have access to the medications you need.
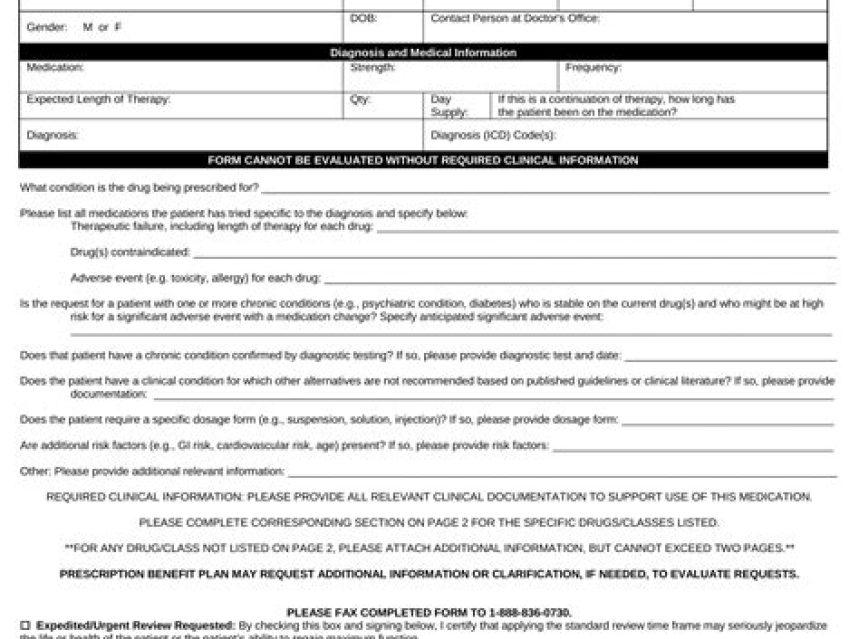
Filling Out the Cvs Caremark Prior Authorization Form
When it comes to filling out the Cvs Caremark Prior Authorization Form, it’s important to pay attention to the details to ensure that the process goes smoothly. Start by carefully reading through the form and following the instructions provided. Make sure to provide all the necessary information, including your personal details, insurance information, and the specific medication or treatment that requires authorization.
Next, take your time to fill out the form accurately and legibly. Double-check the information to avoid any errors or discrepancies, as these could lead to delays in the authorization process. If you have any questions or concerns about certain sections of the form, don’t hesitate to reach out to Cvs Caremark for assistance.
Once you have completed the form, review it one last time to ensure that all the required fields have been filled out. If everything looks in order, submit the form as instructed by Cvs Caremark. Keep in mind that the authorization process may take some time, so it’s important to stay informed about the progress and follow up if necessary.
By filling out the Cvs Caremark Prior Authorization Form accurately and promptly, you can help expedite the process and access the medication or treatment you need in a timely manner. It’s a crucial step in ensuring that your healthcare needs are met, so take the time to complete the form carefully and thoroughly.
Expected Results and Benefits of Using the Form
When it comes to filling out the Cvs Caremark Prior Authorization Form, many individuals may wonder what the expected results and benefits are of using this form. The primary goal of using this form is to obtain approval from the insurance company for coverage of a specific medication that requires prior authorization. By filling out and submitting the form, patients have the opportunity to gain access to the prescribed medication while minimizing out-of-pocket costs.
One of the main benefits of utilizing the Cvs Caremark Prior Authorization Form is the potential cost savings for the patient. In many cases, obtaining prior authorization for a medication can result in the insurance company covering the cost of the medication, reducing the financial burden on the patient. This can be particularly beneficial for individuals with chronic conditions who require ongoing medication.
In addition to cost savings, using the Cvs Caremark Prior Authorization Form can result in a more seamless approval process for obtaining the prescribed medication. By proactively submitting the form and obtaining approval from the insurance company, patients can avoid delays in accessing their medication and can ensure a smooth transition from the prescription to the pharmacy.
Furthermore, the use of the Cvs Caremark Prior Authorization Form can lead to improved health outcomes for patients. By gaining access to the prescribed medication in a timely manner, patients can effectively manage their condition and prevent potential complications. This can ultimately lead to better overall health and well-being for those utilizing the form.
Frequently Asked Questions
What is a Prior Authorization Form?
A prior authorization form is a document that must be submitted by a healthcare provider to a patient’s insurance company to request coverage for a specific prescription medication or treatment that requires pre-approval.
Reasons for Using Cvs Caremark Prior Authorization Form
The Cvs Caremark prior authorization form is used to ensure that patients receive the appropriate medication or treatment, to prevent unnecessary expenses, and to streamline the approval process for prescription drugs and treatments.
How to Obtain Cvs Caremark Prior Authorization Form
The Cvs Caremark prior authorization form can be obtained from the healthcare provider or directly from the Cvs Caremark website. It is important to fill out the form accurately and completely to expedite the approval process.
Filling Out the Cvs Caremark Prior Authorization Form
When filling out the Cvs Caremark prior authorization form, make sure to provide all necessary information about the patient, healthcare provider, and the prescription medication or treatment being requested. It’s important to include any relevant medical history or other supporting documents.
Expected Results and Benefits of Using the Form
Using the Cvs Caremark prior authorization form can lead to faster approval of prescription medications and treatments, reduce out-of-pocket expenses for patients, and ensure that patients receive the appropriate care prescribed by their healthcare providers.